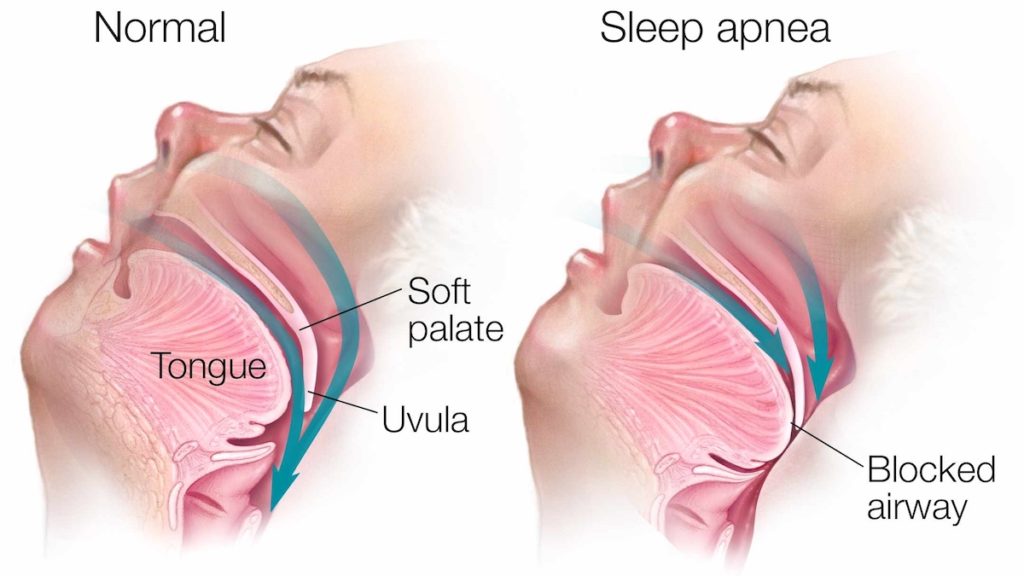
Paediatric sleep disordered breathing or obstructive sleep apnea is a sleep disorder in which your child’s breathing is partially or completely blocked repeatedly during sleep. The condition is due to narrowing or blockage of the upper airway during sleep.
There are differences between paediatric obstructive sleep apnea and adult sleep apnea. While adults usually have daytime sleepiness, children are more likely to have behavioural problems like hyperactivity. The underlying cause in adults is often obesity, while in children the most common underlying cause is poor growth of jaws or enlargement of the adenoids and tonsils.
Early diagnosis and treatment are important to prevent complications that can affect children’s growth, cognitive development and behaviour.
Symptoms
During sleep, signs, and symptoms of pediatric sleep apnea might include:
- Snoring
- Pauses in breathing
- Restless sleep
- Snorting, coughing or choking
- Mouth breathing
- Nighttime sweating
- Bed-wetting
- Sleep terrors
Infants and young children with obstructive sleep apnea don’t always snore. They might just have disturbed sleep.
During the day, children with sleep apnea might:
- Perform poorly in school
- Have difficulty paying attention
- Have learning problems
- Have behavioral problems
- Have poor weight gain
- Be hyperactive
Causes
Obesity is a common factor underlying obstructive sleep apnea in adults. But in children the most common condition leading to obstructive sleep apnea is due to poorly developed jaw or enlarged tonsils and adenoids. However, obesity also plays a role in children. Other underlying factors can be craniofacial anomalies and neuromuscular disorders.
Risk factors
Besides obesity, other risk factors for pediatric sleep apnea include having:
- Down syndrome
- Abnormalities in the jaw, skull or face
- Cerebral palsy
- Sickle cell disease
- Neuromuscular disease
- History of low birth weight
- Family history of obstructive sleep apnea
Complications
Pediatric obstructive sleep apnea can have serious complications, including:
- Failure to grow
- Heart problems
- Sometimes even Death in severe cases.
Diagnosis
To diagnose pediatric sleep apnea, the doctor will review your child’s symptoms and medical history and conduct a physical exam. Your child may have an examination of the neck, mouth and tongue, and adenoids. Your doctor might order several tests to diagnose the condition.
Tests might include:
- Doctors evaluate your child’s condition during an overnight sleep study. This test uses sensors applied to the body to record brain wave activity, breathing patterns, snoring, oxygen levels, heart rate and muscle activity while your child sleeps.
Treatment
Dr Hemant soni specialises in Dental sleep medicine. After thorough evaluation he m ay suggest treatments which may include
- Oral appliances. Oral appliances, such as dental devices or mouthpieces, which help to expand the palate and nasal passages by using techniques of dentofacial orthopaedics, or move your child’s bottom jaw and tongue forward to keep your child’s upper airway open. Expansion and proper positioning of jaws helps in correcting the issue more permanently.
- Myofunctional and breathing Exercises. Breathing can be improved with exercises targeted towards the tissues of throat like soft palate and throat. Various breathing exercises also can help, patient is taught these specific exercises which can also help in improving breathing in sleep.
- Topical nasal steroids or antiallergic medications can help in opening nasal passages temporarily, they can be prescribed by the physician.
- Removal of the tonsils and adenoids.For moderate to severe sleep apnea, we might refer your child to a pediatric ear, nose and throat specialist to discuss removing the tonsils and adenoids. An adenotonsillectomy might improve obstructive sleep apnea by opening the airway. Other forms of upper airway surgery might be recommended, based on the child’s condition.
- Positive airway pressure therapy.In continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BPAP), small machines gently blow air through a tube and mask attached to your child’s nose, or nose and mouth. The machine sends air pressure into the back of your child’s throat to keep your child’s airway open. Doctors often treat pediatric obstructive sleep apnea with positive airway pressure therapy whenother treatments are not effective.
Proper fitting of the mask and refitting as the child grows can help the child tolerate the mask over the face.
CPAP therapy may be needed but is generally avoided as it can affect growth of face when used for long in children.
Book your appointment
